The Science Behind Semaglutide
The Science Behind Semaglutide. Semaglutide is a medication that has been approved for the treatment of type 2 diabetes. It belongs to a class of drugs called GLP-1 receptor agonists, which work by mimicking the effects of a hormone called glucagon-like peptide-1 (GLP-1).
Understanding the science behind semaglutide’s mechanism of action is important because it can help us better understand how the medication works and how it can be used to effectively manage diabetes.
The Role of GLP-1 Receptors in Glucose Regulation
GLP-1 receptors are found on the surface of cells in the pancreas, stomach, and brain. These receptors play a crucial role in regulating glucose levels in the body. When GLP-1 binds to its receptors, it stimulates the release of insulin from pancreatic beta cells, which helps to lower blood sugar levels. GLP-1 also inhibits the release of glucagon, a hormone that raises blood sugar levels. Additionally, GLP-1 slows down the emptying of the stomach, which helps to control appetite and reduce food intake.
GLP-1 receptor agonists like semaglutide work by activating these GLP-1 receptors. By binding to and activating the receptors, semaglutide can mimic the effects of GLP-1 and improve glucose control. This leads to lower blood sugar levels, increased insulin secretion, decreased glucagon secretion, and reduced appetite.
How Semaglutide Activates GLP-1 Receptors
Semaglutide binds to GLP-1 receptors in a similar way to endogenous GLP-1. It has a high affinity for the receptors, meaning that it binds strongly and effectively activates them. Once semaglutide is bound to the receptors, it triggers a series of intracellular signaling events that lead to increased insulin secretion, decreased glucagon secretion, and reduced appetite.
Compared to other GLP-1 receptor agonists, semaglutide has a longer half-life, which means that it stays in the body for a longer period of time. This allows for once-weekly dosing, which can improve patient adherence to the medication. Semaglutide also has a higher potency than other GLP-1 receptor agonists, meaning that it is more effective at activating the receptors and producing the desired effects.
Effects of Semaglutide on Insulin Secretion
Semaglutide Science
One of the main effects of semaglutide is its ability to increase insulin secretion. When semaglutide activates GLP-1 receptors on pancreatic beta cells, it triggers a signaling cascade that leads to the release of insulin. This helps to lower blood sugar levels and improve glucose control.
Compared to other diabetes medications that increase insulin secretion, such as sulfonylureas, semaglutide has a lower risk of causing hypoglycemia (low blood sugar). This is because semaglutide only increases insulin secretion in the presence of high blood sugar levels, whereas sulfonylureas can cause insulin release even when blood sugar levels are already low.
Semaglutide and Glucagon Suppression
In addition to increasing insulin secretion, semaglutide also suppresses the release of glucagon. Glucagon is a hormone that raises blood sugar levels by stimulating the liver to release stored glucose. By inhibiting glucagon secretion, semaglutide helps to lower blood sugar levels and improve glucose control.
The suppression of glucagon secretion by semaglutide is important because it helps to prevent excessive glucose production by the liver. In people with type 2 diabetes, the liver often produces too much glucose, contributing to high blood sugar levels. By suppressing glucagon secretion, semaglutide helps to reduce this excessive glucose production and improve overall glucose control.
Semaglutide and Appetite Control
The science behind semaglutide. Another important effect of semaglutide is its ability to affect appetite and satiety. When semaglutide activates GLP-1 receptors in the brain, it triggers a signaling cascade that leads to reduced appetite and increased feelings of fullness. This can help to reduce food intake and promote weight loss.
Compared to other weight loss medications that affect appetite, such as phentermine, semaglutide has a different mechanism of action. Phentermine works by stimulating the release of norepinephrine, a neurotransmitter that suppresses appetite. Semaglutide, on the other hand, works by activating GLP-1 receptors in the brain, which leads to reduced appetite and increased satiety.
The Impact of Semaglutide on Body Weight

Woman After Slim Shot
Clinical trials have shown that semaglutide is effective in promoting weight loss in people with type 2 diabetes. In one study, participants who took semaglutide lost an average of 14.9% of their body weight, compared to 2.4% in the placebo group. This weight loss was sustained over a 68-week period.
The exact mechanism by which semaglutide promotes weight loss is not fully understood, but it is thought to be related to its effects on appetite and satiety. By reducing appetite and increasing feelings of fullness, semaglutide can help to reduce food intake and promote weight loss.
Semaglutide and Cardiovascular Health
In addition to its effects on glucose control and weight loss, semaglutide has also been shown to have cardiovascular benefits. Clinical trials have demonstrated that semaglutide can reduce the risk of major adverse cardiovascular events, such as heart attack and stroke, in people with type 2 diabetes who have established cardiovascular disease.
The exact mechanisms by which semaglutide improves cardiovascular health are not fully understood, but it is thought to be related to its effects on blood pressure, lipid levels, and inflammation. Semaglutide has been shown to reduce blood pressure, improve lipid profiles, and reduce markers of inflammation, all of which are risk factors for cardiovascular disease.
Clinical Trials and Efficacy of Semaglutide
Numerous clinical trials have evaluated the efficacy and safety of semaglutide in the treatment of type 2 diabetes. These trials have consistently shown that semaglutide is effective in improving glucose control, promoting weight loss, and reducing the risk of cardiovascular events.
In one study, participants who took semaglutide experienced significant reductions in HbA1c levels, a measure of long-term blood sugar control, compared to those who took a placebo. Semaglutide also led to greater weight loss and a lower risk of hypoglycemia compared to other diabetes medications.
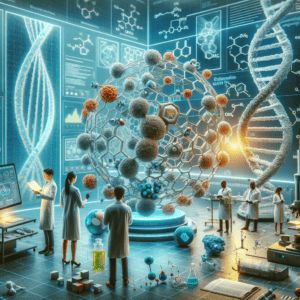
Future Directions for Semaglutide Research
The science behind semaglutide ongoing research is being conducted to further understand the potential uses of semaglutide and other GLP-1 receptor agonists. Some areas of interest include the use of semaglutide in the prevention of type 2 diabetes in high-risk individuals, the treatment of obesity in people without diabetes, and the potential benefits of combining semaglutide with other diabetes medications.
It is important to continue researching and studying semaglutide and other GLP-1 receptor agonists because they have shown great promise in the treatment of type 2 diabetes and related conditions. By understanding the science behind these medications, we can continue to improve their efficacy and safety and develop new treatment options for people with diabetes.
Conclusion of The Science Behind Semaglutide
Semaglutide is a medication that has been approved for the treatment of type 2 diabetes. It works by activating GLP-1 receptors, which leads to improved glucose control, increased insulin secretion, decreased glucagon secretion, reduced appetite, and weight loss. Semaglutide has also been shown to have cardiovascular benefits and is effective in reducing the risk of major adverse cardiovascular events.
Understanding the science behind semaglutide’s mechanism of action is important because it helps us better understand how the medication works and how it can be used to effectively manage diabetes. Ongoing research is being conducted to further explore the potential uses of semaglutide and other GLP-1 receptor agonists. By continuing to study these medications, we can improve their efficacy and safety and develop new treatment options for people with diabetes.